-Anemia of Chronic Disease-
-Anemia of Chronic Disease is typically normocytic, normochromic, and hypoproliferative
-Anemia of chronic disease is thought to primarily be due to a reduction of RBC production by the marrow but may involve a mild shortening of RBC survival
-Many factors are thought to contribute to anemia of chronic disease:
1. Abnormal iron metabolism with reduced absorption of iron for the GI tract and trapping of iron macrophages. This results in reduced plasma levels making iron unavailable for manufacturing new hemoglobin.
2. Inability to increase erythropoiesis due to anemia. Serum EPO levels are mildly increased but there is no response to the marrow, maybe due to increased apoptotic death of RBC precursors in the bone marrow
3. A relative decrease in EPO production. The inverse relationship between hemoglobin levels and serum EPO levels in most anemic conditions is not seen in anemia of chronic disease
4. Shortening lifespan of RBC due to acute inflammation characterized by increased erythrophagocytosis
-Acute event variant of anemia of chronic disease is seen in cases of surgery, trauma, myocardial infarction, sepsis shows many features of anemia of chronic disease (low serum iron, high ferritin, and blunted response to EPO)
-Preferred treatment of anemia of chronic disease is treatment of the underlying disorder rather than replacement therapy with RBC transfusions
-Most anemia of chronic disease have mild anemia with no symptoms
-In some instances high doses of EPO can overcome bone marrow responsiveness in anemia of chronic disease
-Aplastic Anemia-
-Aplastic Anemia is characterized by diminished or absent hematopoietic precursors in the bone marrow
-Aplastic Anemia is often due to injury of the pluripotent stem cell
-Aplastic anemia results in peripheral pancytopenia and bone marrow aplasia
-Stem cell failure can be acquired or congenital (Fanconi Anemia)
-Causes of acquired stem cell aplastic anemia include drugs, chemicals, ionization radiation, and some viruses.
-Aplastic anemia can occur in some immune disorders and occasionally in pregnancy
-Pregnancy associated aplastic anemia is usually self limited and ends with delivery
-Some medications that can cause aplastic anemia include some NSAIDS, choramphenicol, tegretol, dilantin, depakote, and nifedipine
-Many patients with aplastic anemia seek medical attention because of fatigue and cardiopulmonary compromise.
-Other presentations of aplastic anemia include recurrent infections due to neutropenia or mucosal bleeding due to thrombocytopenia (more common)
-Lab workup reveals pancytopenia, along with a reduction in the absolute number of reticulocytes
-Diagnosis can be confirmed with bone marrow biopsy:
1. Bone marrow profoundly hypocellular
2. Infiltration with bone marrow with malignant cells or fibrosis is not present. Usually fat cells and marrow stroma
3. Residual hematopoietic cells are morphologic normal and hematopoiesis is not megaloblastic
-If patients with severe aplastic anemia or very severe aplastic anemia are not treated, 70 percent are dead with 1 year.
-Treatment of aplastic anemia includes: withdrawing any potential offending agents, supportive care with transfusions and antibiotics, and some form of definitive treatment with hematopoietic stem cell transplantation
-ATG (antithymocyte globulin) and cyclosporin is sometimes used in some instances
-Folate Deficiency Anemia-
-Presents as a macrocytic (megaloblastic) anemia
-The most common cause of folate deficiency is nutritional due to malnutrition or alcoholism.
-Older patients are often folic acid deficient
- Alcohol abuse produces a fall in folate within 2-4 days impairing its enterohepatic cycle and inhibiting absorption
-Pregnancy and lactation increase the need for folic acid up to a daily requirement of 800 mcg from 400 mcg
-Several meds interfere with folic acid metabolism: trimethoprim, daraprim, methotrexate, and dilantin
-Hereditary Folate Malabsorption is rare
-Folate deficiency can result in progressive neurologic deterioration early in life
-Can measure serum folate but if megaloblastic anemia can treat empirically
-Usually treated with oral folic acid 1 to 5 mg/ day for 1-4 months or until complete hematologic recovery
-G6PD Deficiency-
-Glucose 6-Phosphate Dehydrogenase (G6PD) deficiency is the an X linked disorder
-G6PD helps maintain the integrity of the RBC
-G6PD is the most common enzymatic disorder of RBC in humans
-The activity of G6PD deficiency was identified as one of the enzymes needed to maintain adequate glutahione (GSH) levels which is found in individuals with acute hemolytic anemia following use of medications.
-The forms of G6PD variants are seen a spectrum of syndromes: acute hemolytic anemia, favism, congenital nonspherocytic anemia, and neonatal hyperbilirubinemia
-Most patients who get hemolytic anemia with G6PD deficiency are asymptomatic in the steady state. The sudden destruction of enzyme deficiency erythrocytes can be triggered by certain chemicals, infections, and rarely metabolic abnormalities such as DKA
-Infections such as salmonella, E. Coli, beta hemolytic streptococci, ricketsiae, and viral hepatitis can incite hemolysis in G6PD deficient patients.
-DKA is capable of triggering destruction in G6PD deficient patients. This is likely secondary to hyperglycemia and acidosis
-Favism most often results from ingestion of fresh Fava beans. Individuals that develop favism are deficiency. Patients get headache, nausea, chills, back pain, and fever following hemoglobinuria and and jaundice. These patients need transfused.
-Patients with congenital nonsphereocytic hemolytic anemia have severe G6PD deficiency that lifelong hemolysis occurs in the absence of drug exposure or infection
-Neonatal hyperbilirubinemia results due to G6PD deficiency in more jaundice then anemia and the anemia is rarely severe. It presents usually on the 2nd or 3rd day of life
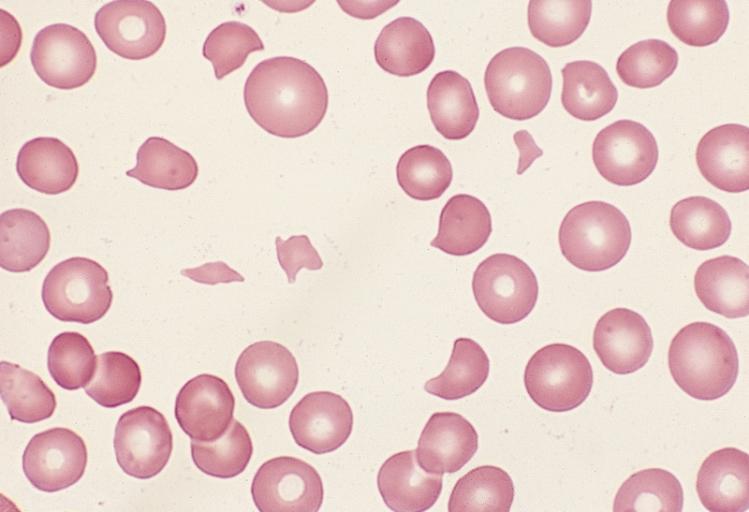
-Diagnostically you get oxidant injury to hemoglobin that leads to methehemoglobin and then to sulfhemoglobin or denatured globulin. This leads to "Bite Cells or Blister Cells"
-Heinz Bodies are brilliant cresyl blue supravital stains reveal denatured globulin
-G6PD deficiency should be considered in the differential diagnosis in any non immune hemolytic anemia
-Treatment of G6PD deficiency should start with avoidance of any triggers of the hemolytic event
-Low dose Primaquine can be beneficial in some instances
-Vitamin E and splenectomy have been tried because of the antioxidant activity with some improvement
-General screening for G6PD has not been developed most often diagnosis is confirmed by peripheral blood smear
-Hemolytic Anemia-
-Hemolytic anemia is defined as anemia due to a shortened survival of circulating RBC
-Hemolysis is shortening of RBC survival to a value of less than 100 days
-A major finding in hemolytic anemia is an increase in the reticulocyte percentage and absolute reticulocyte count
-There are intrinsic (intracorpuscular) and extrinsic causes of hemolysis
-Intrinsic causes of hemolytic anemia with the exception of paroxysmal nocturnal hemoglobinuria and rare condition called acquired alpha thalassemia the intrinsic causes are hereditary
-Destruction of the RBC within the intravascular space requires structure damage to the membrane, examples include: direct trauma, shear stress, heat damage, complement induced lysis, osmotic lysis, lysis from bacterial toxins, lysis from exposures to high concentrations of copper
-Extravascular hemolysis usually occurs with those coated with complement, are destroyed by liver, and receives a larger cardiac output than the spleen.
-Patients with hemolytic anemia present with rapid onset of pallor and anemia, jaundice, history of pigmented gallstones, splenomegaly, presence of spherocytic RBC, RBC shape changes, increased serum lactate dehydrogenase, reduced or absent level of serum haptoglobin, a positive direct anti globulin test (Coombs test) and increased reticulocyte percentage or absolute reticulocyte number
-Lab workup should include: CBC, Reticulocyte count, hepatic function including direct and indirect bilirubin, LDH, haptoglobin, Coombs test, and serum/urine free hemoglobin in urinary hemosiderin if intravascular hemolysis is suspected.
-RBC abnormalities suspicious for hemolysis on peripheral smear include the following: spherocytes, schistocytes, helmet cells, acanthocytes, blister or bite cells, RBC with inclusions (as in malaria), teardrop RBC, Red Cell Ghosts, and prominent basophilic stippling
-Iron Deficiency Anemia-
-presents as a microcytic hypochromic anemia
-with iron deficiency anemia, serum iron is reduced, the level of transferrin and TIBC is elevated
-25 percent of the worlds population is anemic and half of this population is due to iron deficiency anemia
-Most common in preschool children and women
-Reduced availability of iron is the most important cause of anemia due to impaired erythropoiesis
-There are two major causes of iron restricted erythropoiesis
1. Absolute Iron Deficiency-iron stores in the bone marrow and other parts of the monocyte macrophage system in the spleen and liver are absent. Can result from poor intake of iron, reduced iron absorption, and increased blood loss
2. Functional Iron Deficiency-with this there is insufficient availability of iron (low plasma iron levels and/or low transferrin saturation) for incorporation into erythroid precursors with normal or increased body iron stores. This is the case of anemia of chronic disease (inflammation) or treatment with EPO for those patients with renal failure
-Causes of Iron Deficiency-
1. Blood loss
2. Decreased Iron Absorption (Celiac diseases or foods and medications blocking)
3. Intravascular Hemolysis
4. Pulmonary Hemosiderosis (Chronic Pulmonary Hemorrhage)
5. Response to Erythropoietin
6. Gastric Bypass for Morbid Obesity
7. Congenital Iron Deficiency
-Clinical Symptoms include weakness, headache, irritability, and degrees of fatigue and exercise intolerance
-A presumptive diagnosis of iron deficiency anemia is made when there is a positive response of a trial of oral iron therapy.
-A positive response is a modest reticulocyte increase after 5-7 days and an increase in hemoglobin at a rate of approximately 2-4 g/dL every 3-4 weeks until hemoglobin is normal
-If there is no adequate response to iron trial may consider other diagnosis such as sprue, atrophic gastritis, gastrectomy, and from gastric bypass procedures. May need IV iron treatments
-Other indications for parenteral iron include excessive continued blood loss, inflammatory bowel disease, chronic kidney disease, cancer patients, and heart failure patients.
-Bleeding Scan can assess for blood loss source
-Serum or plasma ferritin has replaced assessment of bone marrow stores for the diagnosis of absolute iron deficiency
-Need to consider malignancy or chronic kidney disease with microcytic hypochromic iron deficiency anemia
-Sickle Cell Anemia-
-Sickle Cell Disease is a vaso-occlusive phenomena and it causes hemolysis
-Sickle Cell Disease is an inherited disorder due to homozygous abnormal hemoglobin S (Hb S)
-Vasooclusion results in recurrent painful episodes (sickle cell crisis)
-The term sickle cell disease refers to all conditions associated with sickling, whereas sickle cell anemia describes the homozygous for hemoglobin S
-Patients with sickle beta thalassemia, the disease varies with the quantity of hemoglobin A, often being quite severe in patients with hemoglobin beta (0) thalassemia, and less severe in patients with sickle cell beta (+) thalassemia
-Among patients with coexisting alpha thalassemia, the anemia is less severe but the effects on clinical manifestations are variable
-Episodes of acute pain are the most common type of vasooclusive event and is the most common symptom after the age of 2. Pain can be precipitated by weather conditions, dehydration, stress, menses, alcohol consumption, nocturnal hypoxemia, and rare obstructive sleep apnea.
-Half of vasooclusive have objective findings such as fever, swelling, tenderness, tachypnea, hypertension, nausea, and vomiting
-There is no test to diagnose a vasooclusive event. The peripheral blood smear typically reveals that 5-50 percent of RBC that are reversible sickled cells
-Approximately 24 percent of individuals may suffer an overt stroke with sickle cell anemia by age of 45
-Multiorgan failure is most often seen during severe pain episodes in patients with sickle cell disease
-Reduced (hyposplenism) or absent splenic function is most commonly seen in subjects with sickle cell disease due to repeated infarction. Children are susceptible to life threatening infections (Strep Pneumonia) and should be covered with rocephin parenterally
-Other complications of sickle cell disease include: susceptibility to H. Influenza Type B, Meningitis, Bacterial Pneumonia, Osteomyelitis, bone infarction, and CVA
-Leg ulcers are a frequent complication of sickle cell disease
-Other complications include acute hepatic ischemia, benign cholestasis, hepatic sequestration crisis, transfusional iron overload, acute on chronic cholelithiasis with pigmented stones, drug toxicity, priapism, pulmonary complications, renal complications, retinopathy, and acute chest syndrome
-On lab evaluation will see mild to moderate anemia, increased reticulocytes, unconjugated hyperbilirubinemia, elevated LDH, and low serum haptoglobin.
-All individuals should receive appropriate vaccinations including these for strep pneumonia, influenza, neisseria meningitis, and HIB vaccine
-All individuals should receive folic acid supplementation. Most symptomatic patients should be treated with hydroxyurea.
-During an acute pain episode patients should be treated with IV fluids, oxygen and opioid analgesics
-Thalassemia-
-Vitamin B12 Deficiency-
-Vitamin B 12 Deficiency is dependent on dietary intake, stomach acid, and intrinsic factor in stomach to liberate Vitamin B12 from binding proteins, pancreatic proteases to free Vitamin B12 from binding R factors, secretion of intrinsic factor by gastric parietal cells to bind Vitamin B 12, and an intact ileum with functional receptors
-Causes of Vitamin B 12 Deficiency include pernicious anemia, autoimmune metaplastic atrophic gastritis, autoantibody formation against intrinsic factor, gastrectomy, gastritis, tapeworm, drugs, inadequate dietary intake, HIV infection, Nitrous oxide exposure, and H. Pylori infection, and hereditary problems
-Clinical manifestations include macrocytic anemia
-Only Vitamin B 12 deficiency produces neurologic changes not folate deficiency
-Neurologic changes include neuropathy, degeneration of the dorsal an lateral spine columns, weakness, spasticity, clonus, paraplegia, and even fecal and urinary incontinence can occur from deficiency
-Vitamin B 12 deficiency increases risk for osteoporosis
-Treatment involves depo preparation of Vitamin B 12 once a month and exploring possible correctable etiology
-Several meds interfere with folic acid metabolism: trimethoprim, daraprim, methotrexate, and dilantin
-Hereditary Folate Malabsorption is rare
-Folate deficiency can result in progressive neurologic deterioration early in life
-Can measure serum folate but if megaloblastic anemia can treat empirically
-Usually treated with oral folic acid 1 to 5 mg/ day for 1-4 months or until complete hematologic recovery
-G6PD Deficiency-
-Glucose 6-Phosphate Dehydrogenase (G6PD) deficiency is the an X linked disorder
-G6PD helps maintain the integrity of the RBC
-G6PD is the most common enzymatic disorder of RBC in humans
-The activity of G6PD deficiency was identified as one of the enzymes needed to maintain adequate glutahione (GSH) levels which is found in individuals with acute hemolytic anemia following use of medications.
-The forms of G6PD variants are seen a spectrum of syndromes: acute hemolytic anemia, favism, congenital nonspherocytic anemia, and neonatal hyperbilirubinemia
-Most patients who get hemolytic anemia with G6PD deficiency are asymptomatic in the steady state. The sudden destruction of enzyme deficiency erythrocytes can be triggered by certain chemicals, infections, and rarely metabolic abnormalities such as DKA
-Infections such as salmonella, E. Coli, beta hemolytic streptococci, ricketsiae, and viral hepatitis can incite hemolysis in G6PD deficient patients.
-DKA is capable of triggering destruction in G6PD deficient patients. This is likely secondary to hyperglycemia and acidosis
-Favism most often results from ingestion of fresh Fava beans. Individuals that develop favism are deficiency. Patients get headache, nausea, chills, back pain, and fever following hemoglobinuria and and jaundice. These patients need transfused.
-Patients with congenital nonsphereocytic hemolytic anemia have severe G6PD deficiency that lifelong hemolysis occurs in the absence of drug exposure or infection
-Neonatal hyperbilirubinemia results due to G6PD deficiency in more jaundice then anemia and the anemia is rarely severe. It presents usually on the 2nd or 3rd day of life
-Diagnostically you get oxidant injury to hemoglobin that leads to methehemoglobin and then to sulfhemoglobin or denatured globulin. This leads to "Bite Cells or Blister Cells"
-Heinz Bodies are brilliant cresyl blue supravital stains reveal denatured globulin
-G6PD deficiency should be considered in the differential diagnosis in any non immune hemolytic anemia
-Treatment of G6PD deficiency should start with avoidance of any triggers of the hemolytic event
-Low dose Primaquine can be beneficial in some instances
-Vitamin E and splenectomy have been tried because of the antioxidant activity with some improvement
-General screening for G6PD has not been developed most often diagnosis is confirmed by peripheral blood smear
-Hemolytic Anemia-
-Hemolysis is shortening of RBC survival to a value of less than 100 days
-A major finding in hemolytic anemia is an increase in the reticulocyte percentage and absolute reticulocyte count
-There are intrinsic (intracorpuscular) and extrinsic causes of hemolysis
-Intrinsic causes of hemolytic anemia with the exception of paroxysmal nocturnal hemoglobinuria and rare condition called acquired alpha thalassemia the intrinsic causes are hereditary
-Destruction of the RBC within the intravascular space requires structure damage to the membrane, examples include: direct trauma, shear stress, heat damage, complement induced lysis, osmotic lysis, lysis from bacterial toxins, lysis from exposures to high concentrations of copper
-Extravascular hemolysis usually occurs with those coated with complement, are destroyed by liver, and receives a larger cardiac output than the spleen.
-Patients with hemolytic anemia present with rapid onset of pallor and anemia, jaundice, history of pigmented gallstones, splenomegaly, presence of spherocytic RBC, RBC shape changes, increased serum lactate dehydrogenase, reduced or absent level of serum haptoglobin, a positive direct anti globulin test (Coombs test) and increased reticulocyte percentage or absolute reticulocyte number
-Lab workup should include: CBC, Reticulocyte count, hepatic function including direct and indirect bilirubin, LDH, haptoglobin, Coombs test, and serum/urine free hemoglobin in urinary hemosiderin if intravascular hemolysis is suspected.
-RBC abnormalities suspicious for hemolysis on peripheral smear include the following: spherocytes, schistocytes, helmet cells, acanthocytes, blister or bite cells, RBC with inclusions (as in malaria), teardrop RBC, Red Cell Ghosts, and prominent basophilic stippling
-Iron Deficiency Anemia-
-presents as a microcytic hypochromic anemia
-with iron deficiency anemia, serum iron is reduced, the level of transferrin and TIBC is elevated
-25 percent of the worlds population is anemic and half of this population is due to iron deficiency anemia
-Most common in preschool children and women
-Reduced availability of iron is the most important cause of anemia due to impaired erythropoiesis
-There are two major causes of iron restricted erythropoiesis
1. Absolute Iron Deficiency-iron stores in the bone marrow and other parts of the monocyte macrophage system in the spleen and liver are absent. Can result from poor intake of iron, reduced iron absorption, and increased blood loss
2. Functional Iron Deficiency-with this there is insufficient availability of iron (low plasma iron levels and/or low transferrin saturation) for incorporation into erythroid precursors with normal or increased body iron stores. This is the case of anemia of chronic disease (inflammation) or treatment with EPO for those patients with renal failure
-Causes of Iron Deficiency-
1. Blood loss
2. Decreased Iron Absorption (Celiac diseases or foods and medications blocking)
3. Intravascular Hemolysis
4. Pulmonary Hemosiderosis (Chronic Pulmonary Hemorrhage)
5. Response to Erythropoietin
6. Gastric Bypass for Morbid Obesity
7. Congenital Iron Deficiency
-Clinical Symptoms include weakness, headache, irritability, and degrees of fatigue and exercise intolerance
-A presumptive diagnosis of iron deficiency anemia is made when there is a positive response of a trial of oral iron therapy.
-A positive response is a modest reticulocyte increase after 5-7 days and an increase in hemoglobin at a rate of approximately 2-4 g/dL every 3-4 weeks until hemoglobin is normal
-If there is no adequate response to iron trial may consider other diagnosis such as sprue, atrophic gastritis, gastrectomy, and from gastric bypass procedures. May need IV iron treatments
-Other indications for parenteral iron include excessive continued blood loss, inflammatory bowel disease, chronic kidney disease, cancer patients, and heart failure patients.
-Bleeding Scan can assess for blood loss source
-Serum or plasma ferritin has replaced assessment of bone marrow stores for the diagnosis of absolute iron deficiency
-Need to consider malignancy or chronic kidney disease with microcytic hypochromic iron deficiency anemia
-Sickle Cell Anemia-
-Sickle Cell Disease is a vaso-occlusive phenomena and it causes hemolysis
-Sickle Cell Disease is an inherited disorder due to homozygous abnormal hemoglobin S (Hb S)
-Vasooclusion results in recurrent painful episodes (sickle cell crisis)
-The term sickle cell disease refers to all conditions associated with sickling, whereas sickle cell anemia describes the homozygous for hemoglobin S
-Patients with sickle beta thalassemia, the disease varies with the quantity of hemoglobin A, often being quite severe in patients with hemoglobin beta (0) thalassemia, and less severe in patients with sickle cell beta (+) thalassemia
-Among patients with coexisting alpha thalassemia, the anemia is less severe but the effects on clinical manifestations are variable
-Episodes of acute pain are the most common type of vasooclusive event and is the most common symptom after the age of 2. Pain can be precipitated by weather conditions, dehydration, stress, menses, alcohol consumption, nocturnal hypoxemia, and rare obstructive sleep apnea.
-Half of vasooclusive have objective findings such as fever, swelling, tenderness, tachypnea, hypertension, nausea, and vomiting
-There is no test to diagnose a vasooclusive event. The peripheral blood smear typically reveals that 5-50 percent of RBC that are reversible sickled cells
-Approximately 24 percent of individuals may suffer an overt stroke with sickle cell anemia by age of 45
-Multiorgan failure is most often seen during severe pain episodes in patients with sickle cell disease
-Reduced (hyposplenism) or absent splenic function is most commonly seen in subjects with sickle cell disease due to repeated infarction. Children are susceptible to life threatening infections (Strep Pneumonia) and should be covered with rocephin parenterally
-Other complications of sickle cell disease include: susceptibility to H. Influenza Type B, Meningitis, Bacterial Pneumonia, Osteomyelitis, bone infarction, and CVA
-Leg ulcers are a frequent complication of sickle cell disease
-Other complications include acute hepatic ischemia, benign cholestasis, hepatic sequestration crisis, transfusional iron overload, acute on chronic cholelithiasis with pigmented stones, drug toxicity, priapism, pulmonary complications, renal complications, retinopathy, and acute chest syndrome
-On lab evaluation will see mild to moderate anemia, increased reticulocytes, unconjugated hyperbilirubinemia, elevated LDH, and low serum haptoglobin.
-All individuals should receive appropriate vaccinations including these for strep pneumonia, influenza, neisseria meningitis, and HIB vaccine
-All individuals should receive folic acid supplementation. Most symptomatic patients should be treated with hydroxyurea.
-During an acute pain episode patients should be treated with IV fluids, oxygen and opioid analgesics
-Thalassemia-
-Thalassemia refers to a spectrum of diseases characterized by reduced or absent production of one or more globin chains
-The majority of patients with alpha and beta thalassemia minor are asymptomatic and may be diagnosed because of microcytic hypochromic anemia
-Thalassemia of intermediate degrees of severity (thalassemia intermedia) are common throughout the world and may be due to the presence of more one hemoglobin mutation in the same patient or presence of an abnormal hemoglobin with a reduced production rate
-Beta thalassemia major and alpha thalassemia major are at the other end of the spectrum. Beta thalassemia major are associated with lifelong transfusion dependent anemia. Alpha is not compatible with extrauterine life
-Patients with Beta Thalassemia Major suffer from severe chronic anemia, chronic hemolysis, organ damage associated with iron overload, and profound local and systemic effects of a rapidly and relentless expanding mass of bone marrow progenitors
-Clinical manifestations of Beta Thalassemia Major include skeletal changes, hepatomegaly, Splenomegaly, Enlarged Kidneys (because of hematopoiesis), hypogonadism, growth failure, diabetes, and hypothyroidism
-Cardiac manifestations include heart failure and fatal arrhythmias are a manifestation of Beta Thalassemia Major
-Lab findings include profound hypochromic, microcytic anemia with bizarre morphology (Heinz Bodies)
-Iron level is usually elevated because of the high rate of RBC turnover, transferrin and TIBC is elevated
-Increased unconjugated bilirubin and LDH and low levels of haptoglobin are seen with Beta Thalassemia Major
-Diagnosis of Beta Thalassemia Major will be made in all patients around 6-12 months due to the presence of pallor, irritability, growth retardation, and abdominal swelling due to hepatomegaly and jaundice
-Vitamin B12 Deficiency-
-Vitamin B 12 Deficiency is dependent on dietary intake, stomach acid, and intrinsic factor in stomach to liberate Vitamin B12 from binding proteins, pancreatic proteases to free Vitamin B12 from binding R factors, secretion of intrinsic factor by gastric parietal cells to bind Vitamin B 12, and an intact ileum with functional receptors
-Causes of Vitamin B 12 Deficiency include pernicious anemia, autoimmune metaplastic atrophic gastritis, autoantibody formation against intrinsic factor, gastrectomy, gastritis, tapeworm, drugs, inadequate dietary intake, HIV infection, Nitrous oxide exposure, and H. Pylori infection, and hereditary problems
-Clinical manifestations include macrocytic anemia
-Only Vitamin B 12 deficiency produces neurologic changes not folate deficiency
-Neurologic changes include neuropathy, degeneration of the dorsal an lateral spine columns, weakness, spasticity, clonus, paraplegia, and even fecal and urinary incontinence can occur from deficiency
-Vitamin B 12 deficiency increases risk for osteoporosis
-Treatment involves depo preparation of Vitamin B 12 once a month and exploring possible correctable etiology





Most prostate cancers are adenocarcinomas, cancers that arise in glandular cells of the prostate’s epithelial tissue. Prostate cancers usually progress slowly and produce no symptoms in the initial stages. Eventually, the tumor may enlarge like mine too, the prostate gland, pressing on the urethra and causing painful or frequent urination and blood in the urine. So I was so uncomfortable with this prostate cancer diseases then I decided to do online search on how to cure cancer because I well have read a lot about herbal medicine, I came across a lot of testimony how Dr Itua cure HIV/herpes then Cancer was listed below the comment.with courage I contacted Dr Itua and he sent me his herbal medicine through Courier service then I was asked to pick it up at my post office which i quickly did. I contacted Dr Itua that I have received my herbal medicine so he instructed me on how to drink it for three weeks and that is how Dr Itua Herbal Medicine cures my prostate Cancer, The treatment takes three weeks and I was cured completely. Dr Itua is a god sent and I thank him every day of my life. Contact him now On: Email:drituaherbalcenter@gmail.com/ Whatsapp:+2348149277967.
ReplyDeleteHe listed that he can as well cure the following diseases below.... Cerebral Amides. Lung Cancer,Brain cancer,Esophageal cancer,Gallbladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma Intestinal cancer,Kidney cancer,Leukemia,Liver cancer,Melanoma,Mesothelioma,Multiple myeloma,Neuroendocrine tumors,Hodgkin lymphoma,Oral cancer,Ovarian cancer,Sinus cancer,Soft tissue sarcoma,Spinal cancer,Stomach cancer,Meniere's disease , Testicular cancer,Throat cancer,Thyroid Cancer,Uterine cancer,Vaginal cancer,Vulvar cancer. Alzheimer's disease,Autism,measles, tetanus, whooping cough, tuberculosis, polio and diphtheria Adrenocortical carcinoma. Alma, Uterine Cancer, Breast Cancer, Allergic diseases. Kidney cancer, Love Spell, Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Generalized dermatitis,Alzheimer's disease,Brain Tumor,Lupus,Endometrial Cancer, cerebrovascular diseases
Dementia.Colo rectal cancer, Lottery Spell, Bladder Cancer, Skin Cancer,Ovarian Cancer,Pancreatic Cancer, HIV /Aids,Brain Tumor, Herpes, Non-Hodgkin lymphoma, Inflammatory bowel disease, Copd, Diabetes, Hepatitis