-Acute/Chronic Lymphocytic Leukemia-
-Acute Leukemia is the most common form of cancer in children (30 percent of all children malignancies)
-Acute Lymphocytic Leukemia (ALL) is 5 times more common than AML
-The overall survival rate is 85% with ALL
-The most common presenting symptoms of ALL are fever, bleeding, bone pain, and lymphadenopathy.
-Most children with ALL with have anemia and/or thrombocytopenia with normal or depressed WBC
-Bone marrow biopsy is indicated if atypical cells are found in peripheral blood, use explained depression of more than one peripheral blood element, or unexplained lymphadenopathy or hepatosplenomegaly with associated cytopenias
-The diagnosis of CNS leukemia requires confirmation of leukemic cells in the CSF
-Treatment protocols are multi drug and divided into phases of induction, consolidation, and maintenance
-Most treatment protocols take 2-3 years to complete
-There is therapy also directed at the central nervous system
-Chronic Lymphocytic Leukemia (CLL)-
-B Cell Chronic Lymphocytic Leukemia is considered to be identical to the mature B cell neoplasm small lymphocytic leukemia
-CLL is characterized by a accumulation of functionally incompetent lymphocytes which are monoclonal in origin
-Most patients present with painless generalized lymphadenopathy which has been present usually for years
-Hepatosplenomegaly and extranodal infiltrates may be seen
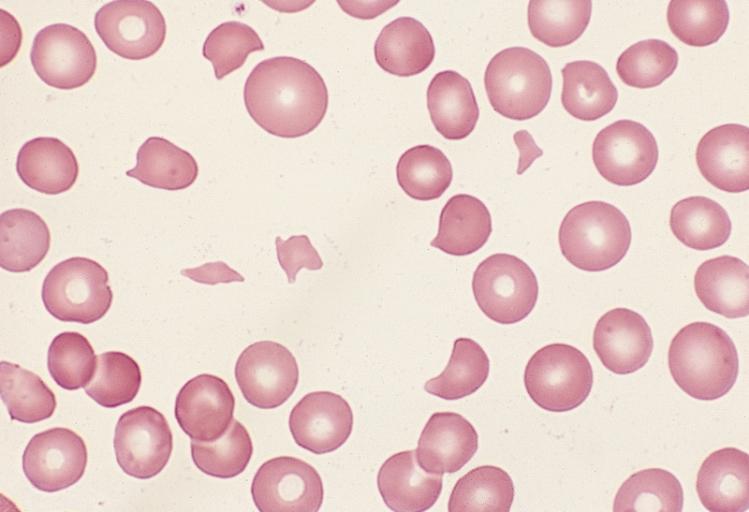
-Patients on the peripheral blood smear with normal or mild lymphocytosis but will have an absolute lymphocyte count of less than 5000/microL
-A serum paraprotein or hypogammaglobulinemia is found in 20-40 percent of the cases
-Patients with CLL patients may develop autoimmune hemolytic anemia, pure red cell aplasia, and autoimmune thrombocytopenia
-Elevations of LDH and Beta 2 microglobulin may occur
-Not all patients with CLL require treatment at the time of diagnosis. CLL is heterogenous disease and some have survival rates similar to the normal population without treatment. With the exception of allogenic cell transplant CLL cannot be cured by current treatment options. Spontaneous regression of variable duration is a rare occurrence
-Most patients with CLL undergoing chemotherapy will have an initial complete or partial response, except those getting a allogenic cell transplantation
-Acute/Chronic Myelogenous Leukemia-
-Acute Myelogenous Leukemia (AML, acute non lymphocytic leukemia) is group of well defined neoplasms having precursor cells committed to the myeloid line of cellular development
-There is an accumulation of leukemic blast cells or immature forms in the bone marrow in the peripheral blood and sometimes in other tissues
-The increased production of these malignant cells results in systemic sequelae including anemia, bleeding and increased risk of infection
-The cells that AML gives rise to include granulocytic, monocytic, erythroid, or megakaryocytic elements
-Patients with AML present usually with pancytopenia, weakness, and fatigue, infections, bleeding, or bruising
-Bone pain is infrequent with AML. Palpable significant lymphadenopathy is rare
-Bone marrow aspiration and biopsy is a key component to diagnosis of AML. The bone marrow is usually hypercellular with partial or a total replacement of normal cellular components with immature or undifferentiated cells.
-A presumptive diagnosis of AML can be made when there is circulating leukemic blast int he peripheral blood smear. Definitive diagnosis requires bone marrow aspiration on biopsy. Blast cells must contain at least 20% of the total cells in the aspirate
-Remission induction is the goal of treatment with patients with AML.
-Treatment is directed at the specific age of the patient and involves chemotherapy most of the time
-Colony stimulating factors are usually not effective
-Treatment with transfusions as well as infections are important for supportive care
-Chronic Myelogenous Leukemia (CML)-
-CML is a myeloproliferative neoplasm characterized by the dysregulated production and uncontrolled proliferation of mature and maturing granulocytes and fairly normal differentiation
-The hallmark of CML is the uncontrolled production of mature and maturing granulocytes, predominately neutrophils, but also basophils and eosinophils
-In the absence of treatment, CML has a triphasic or biphasic clinical course as it progresses to the chronic phase to an accelerated phase on to the terminal blast crisis
-The peripheral smear typically demonstrates a leukocytosis with a median white count of 100,000 microL. The WBC differential typically shows all cells of the neutrophilic series, from myeloblasts to mature neutrophils with peaks in the percent of myelocytes and segmented neutrophils
-Bone marrow aspiration and biopsy demonstrates granulocytic hyperplasia with maturation pattern that reflects the peripheral blood smear
-The diagnosis of CML is suspected by identifying the typical findings in the blood and bone marrow and then confirmed by the demonstration of the Philadelphia Chromosome
-CML has 3 phases; Chronic Stable Phase, Accelerated Phase, and Blast Crisis
-CML has a potential cure with allogenic hematopoietic cell transplantation
-CML can by controlled without cure using tyrosine kinase inhibitors (TKI's)
-CML palliative therapy with cytotoxic agents
-Lymphoma-
-Lymphoma can be characterized as non hodgkin lymphoma (NHL) or hodgkin lymphoma
-Non Hodgkin Lymphoma consists of a diverse group of malignant neoplasms of the lymphoid tissues variously derived from B Cell progenitors, T Cell progenitors, mature B Cells, or mature T Cells
-Most adults have low grade NHL and children is more aggressive
-Potential complications of NHL include: SVC and IVC obstruction, airway obstruction, intestinal obstruction, intussusception, spinal cord compression, pericardial tamponade, lymphomatous meningitis, CNS mass lesions, hyperuricemia, tumor lysis syndrome, urethral obstruction, unilateral or bilateral hydronephrosis and venous thromoboembolic disease
-Symptoms of NHL usually happens over 1-3 weeks. Usually presents with enlarging non tender lymphadenopathy or as symptoms due to compression of surrounding structures such as wheezing, facial swelling, respiratory distress, asymmetric tonsils, or acute abdominal pain
-Hepatosplenomegaly may be present in advanced NHL
-Systemic symptoms such as fever, weight loss, and night sweats (B Symptoms) will be presents in a minority of the patients
-Burkitt Lymphoma can have CNS involvement
-May find unexplained anemia, thrombocytopenia, leukopenia, hyperuricemia, and elevated LDH with NHL
-Radiographs may demonstrate masses or lymphadenopathy in the neck chest or abdomen with NHL
-The diagnosis of NHL is based upon the evaluation of biopsied tissue
-Combination chemotherapy is used primarily with NHL in children. Adults usually have radiation therapy with NHL
-Adults can also get immunotherapy based on the stage of the disease
-Hodgkin Lymphoma has few risk factors that have been convincingly identified such as viral exposure with Epstein Barr Virus.
-Hodgkin Lymphoma is characterized by the presence of Reed Sternberg Cells
-Presenting symptoms of Hodgkins Lymphoma include lymphadenopathy and mediastinal masses. B symptoms (fever, weight loss, and night sweats) are present
-Hepatosplenomegaly may be present with advance Hodgkin Lymphoma
-The diagnosis of Hodgkins Lymphoma is based on tissue biopsy and the presence of Reed Sternberg Cells
-Treatment of Hodgkins Lymphoma may include chemotherapy and/or radiation therapy based on the type and stage
-Multiple Myeloma-
-Multiple Myeloma is characterized by a neoplastic proliferation of a single clone of plasma cells producing monoclonal immunoglobulin
-The clone of plasma cells proliferates in bone marrow and causes extensive skeletal destruction with osteolytic lesions, osteopenia, and/or fractures
-The diagnosis of multiple myeloma is often suspected because of bone pain with lytic lesions on routine films, increased total serum protein and/or presence of monoclonal protein in the urine or serum, unexplained anemia, hypercalcemia, or acute renal failure with a bland urinalysis
-Presenting symptoms include anemia, bone pain, elevated creatinine, fatigue, weakness, hypercalcemia, weight loss, paresthesias, hepatosplenomegaly, or lymphadenopathy
-Monoclonal protein in the serum or urine is a major criteria for the diagnosis of multiple myeloma. Bence Jones proteins are produced 16 percent of the time. Electrophoresis of the urine should be ordered
-Bone Marrow aspirate and biopsy are a key component to the diagnosis of multiple myeloma.
-Main treatment of Multiple Myeloma is chemotherapy. Stem Cell Transplant can be considered for those who treatment fails